
Background:
The survival of patients with chronic myeloid leukemia (CML) in chronic phase (CP) is approaching that of general population particularly in patients who achieved cytogenetic and/or molecular response. However, a proportion of patients on tyrosine kinase inhibitors (TKIs) develop intolerance and/or resistance, and required subsequent TKI therapy. The aims of this study is to evaluate the outcome of patients with CML-CP treated with third-line TKI therapy.
Methods:
We performed a retrospective review of patients with CML-CP or accelerated phase (AP) who received a third-line TKI therapy at out institution. Overall survival was calculated from the start of TKI therapy until death from any cause at any time. Univariate and backward multivariate Cox regression was performed to identify prognostic factors for survival after variable selections by a p value cutoff of 0.250 by univariate analysis. Time to stem cell transplant during the third-line TKI therapy was handled as a time-dependent variable.
Results:
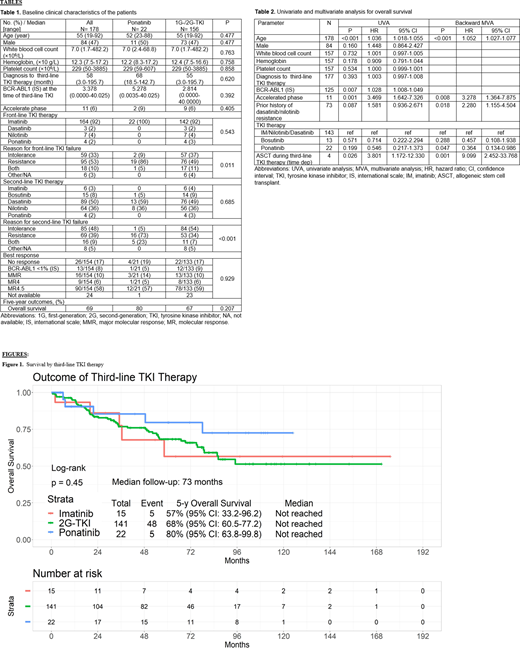
Between March 2005 and November 2015, 178 patients who received 1 third-line TKI therapy were included in the analysis: 65 (64%) patients nilotinib; 63 (35%) dasatinib; 22 (12%) ponatinib; 15 (8%) imatinib; and 13 (7%) bosutinib. Patient characteristics are described in Table1. Among 22 patients on ponatinib, 21 (95%) patients had prior history of resistance to second-generation TKIs. Overall, the median follow-up was 73 months (range, 0.6-175.2) without significant difference by TKI therapy (P=0.260); nilotinib, 78 months; dasatinib, 73 months; ponatinib, 100 months; imatinib, 64 months; bosutinib, 72 months. The median time from the diagnosis of CML-CP to third-line TKI therapy was 58 months (range, 2.96-195.7).
Among 178 patients, 164 (92%) patients received imatinib as the first TKI therapy; 7 (4%), nilotinib; 3 (2%), dasatinib; and 4 (2%), ponatinib. Eighty-nine (50%) received dasatinib as the second TKI therapy; 64 (36%), received nilotinib; 15 (8%), bosutinib; 6 (3%), imatinib; and 4 (2%), ponatinib. Among 154 evaluable patients, 90 (58%) molecular response 4.5 (MR4.5) (BCR-ABL1 ≤0.0032% [IS]); 9 (5%) molecular response 4 (MR4) (BCR-ABL1 ≤0.01% [IS]); 16 (9%) major molecular response (MMR) (BCR-ABL1 ≤0.1% [IS]) 13 (7%), BCR-ABL1 ≤1% (IS); and 26 (15%) had no response.
Of the 178 patients 81 (45%) discontinued TKI therapy due to intolerance and/or resistance. The median duration of the third-line TKI therapy was 9 months (range, 1.0-86.9).
Overall, the median survival was not reached with a 5-year survival rate of 69% (Figure 1). The 5-year survival rates were 57%, 68%, and 80% in patients who received imatinib, second-generation TKIs, and ponatinib, respectively (P=0.45). These 5-year survival rates were 38%, 56%, and 84%, respectively among patients with previous history of resistance to second-generation TKIs (dasatinib, nilotinib, or bosutinib) during the frontline and/or second-line TKI therapy. The median survival were 36 months, 75 months, not reached, respectively (P=0.100).
Backward multivariate analysis identified age (P<0.001; hazard ratio [HR], 1.052; 95% confidence interval [CI], 1.027-1.077), the progression to AP at the time of third-line TKI therapy (P=0.008; HR, 3.278; 95% CI, 1.364-7.875), previous history of resistance to a second-generation TKI therapy (P=0.018; HR, 2.280; 95% CI, 1.155-4.504), and stem cell transplant during the third-line TKI therapy (P=0.001; HR, 9.099; 95% CI, 2.452-33.768) as adverse prognostic factors for survival. In contrast ponatinib therapy as the third-line TKI was the only prognostic factor for favorable survival (P=0.047; HR, 0.364; 95% CI, 0.134-0.986).
Conclusion:
Third-line TKI therapy can achieve an optimal response with long-term survival in patients with CML-CP/-AP. In patients with previous history of resistance to second-generation TKIs, ponatinib is an optimal TKI associated with favorable survival. Allogeneic stem cell transplant should be deferred till patients fail ponatinib therapy.
Sasaki:Novartis: Consultancy, Research Funding; Daiichi Sankyo: Consultancy; Otsuka: Honoraria; Pfizer Japan: Consultancy. Jabbour:BMS: Other: Advisory role, Research Funding; Amgen: Other: Advisory role, Research Funding; Genentech: Other: Advisory role, Research Funding; Pfizer: Other: Advisory role, Research Funding; Takeda: Other: Advisory role, Research Funding; AbbVie: Other: Advisory role, Research Funding; Adaptive Biotechnologies: Other: Advisory role, Research Funding. Issa:Syndax: Research Funding; Celegene: Research Funding; Novartis: Membership on an entity's Board of Directors or advisory committees. Garcia-Manero:Novartis: Research Funding; Merck: Research Funding; Bristol-Myers Squibb: Consultancy, Research Funding; Astex Pharmaceuticals: Consultancy, Honoraria, Research Funding; Genentech: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Helsinn Therapeutics: Consultancy, Honoraria, Research Funding; H3 Biomedicine: Research Funding; AbbVie: Honoraria, Research Funding; Amphivena Therapeutics: Research Funding; Onconova: Research Funding; Celgene: Consultancy, Honoraria, Research Funding; Jazz Pharmaceuticals: Consultancy; Acceleron Pharmaceuticals: Consultancy, Honoraria. Kadia:Novartis: Honoraria; Cyclacel: Research Funding; Astellas: Research Funding; Pulmotec: Research Funding; Astra Zeneca: Research Funding; BMS: Honoraria, Research Funding; Ascentage: Research Funding; Abbvie: Honoraria, Research Funding; JAZZ: Honoraria, Research Funding; Genentech: Honoraria, Research Funding; Incyte: Research Funding; Amgen: Research Funding; Pfizer: Honoraria, Research Funding; Cellenkos: Research Funding; Celgene: Research Funding. Yilmaz:Daicho Sankyo: Research Funding; Pfizer: Research Funding; Pint Pharma: Honoraria. DiNardo:ImmuneOnc: Honoraria; Novartis: Consultancy; Calithera: Research Funding; Jazz: Honoraria; Agios: Consultancy, Honoraria, Research Funding; Notable Labs: Membership on an entity's Board of Directors or advisory committees; Celgene: Consultancy, Honoraria, Research Funding; Daiichi Sankyo: Consultancy, Honoraria, Research Funding; Takeda: Honoraria; AbbVie: Consultancy, Honoraria, Research Funding; Syros: Honoraria; MedImmune: Honoraria. Pemmaraju:Blueprint Medicines: Honoraria; Samus Therapeutics: Research Funding; Incyte Corporation: Honoraria; Daiichi Sankyo: Research Funding; Affymetrix: Other: Grant Support, Research Funding; AbbVie: Honoraria, Research Funding; Stemline Therapeutics: Honoraria, Research Funding; SagerStrong Foundation: Other: Grant Support; Pacylex Pharmaceuticals: Consultancy; Celgene: Honoraria; Novartis: Honoraria, Research Funding; DAVA Oncology: Honoraria; Plexxikon: Research Funding; Roche Diagnostics: Honoraria; LFB Biotechnologies: Honoraria; Cellectis: Research Funding; MustangBio: Honoraria. Cortes:Amphivena Therapeutics: Research Funding; Astellas: Research Funding; Telios: Research Funding; BioPath Holdings: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Merus: Research Funding; Novartis: Consultancy, Research Funding; Jazz Pharmaceuticals: Consultancy, Research Funding; BiolineRx: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding; Arog: Research Funding; Sun Pharma: Research Funding; Takeda: Consultancy, Research Funding; Daiichi Sankyo: Consultancy, Research Funding; Bristol-Myers Squibb: Research Funding; Immunogen: Research Funding. Kantarjian:Amgen: Honoraria, Research Funding; AbbVie: Honoraria, Research Funding; Astex: Research Funding; Agios: Honoraria, Research Funding; Jazz Pharma: Research Funding; Novartis: Research Funding; Ariad: Research Funding; Immunogen: Research Funding; Actinium: Honoraria, Membership on an entity's Board of Directors or advisory committees; Cyclacel: Research Funding; BMS: Research Funding; Takeda: Honoraria; Daiichi-Sankyo: Research Funding; Pfizer: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal